URGENT UPDATE: A team at the University of California Berkeley has just announced a groundbreaking advancement in CRISPR-Cas9 technology, significantly boosting its efficiency for gene editing in human T cells. This development, unveiled in a recent publication, addresses a critical challenge that has limited CRISPR’s therapeutic applications: the ability to effectively transport Cas9 proteins into the cell nucleus.
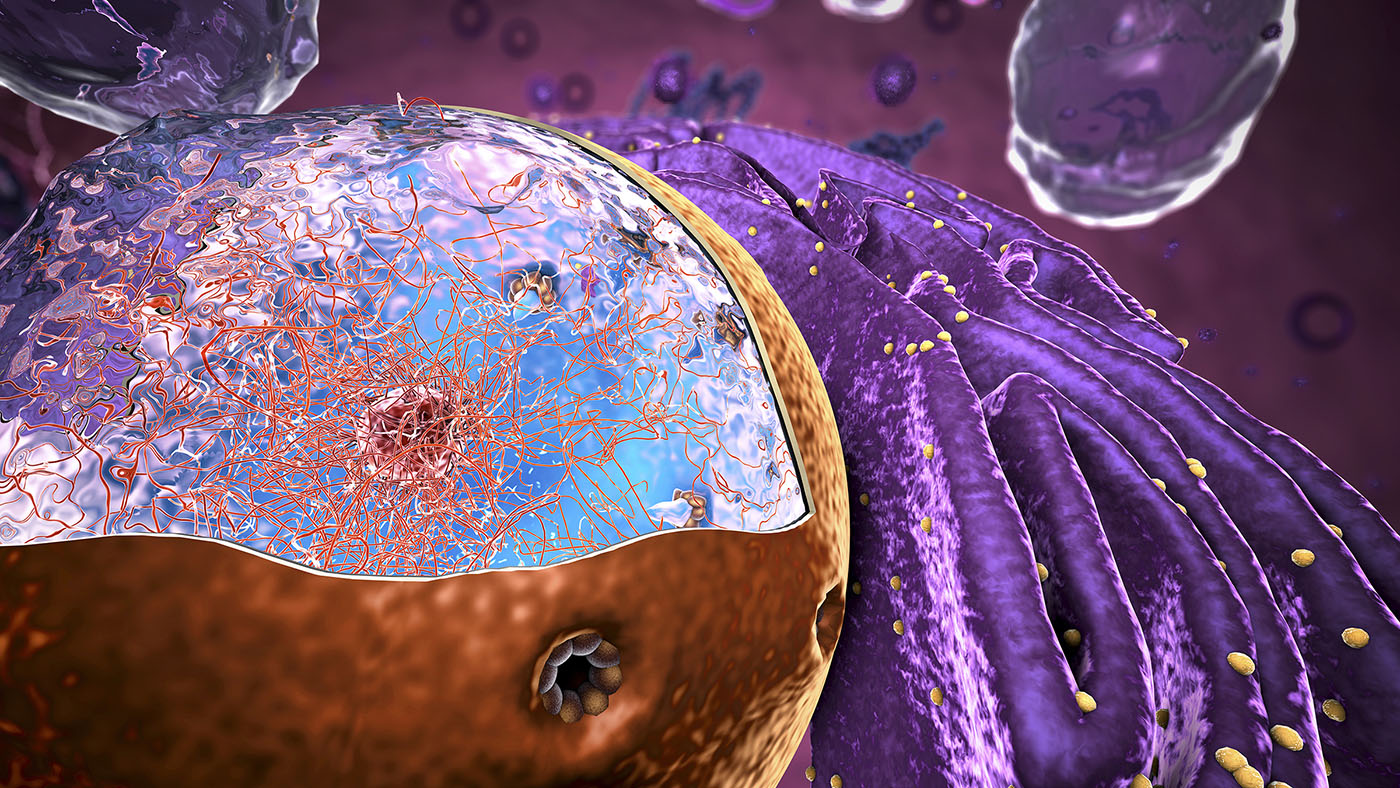
Current methods for delivering CRISPR-Cas9 often result in low nuclear entry rates, reducing the effectiveness of gene editing. Researchers have found that by increasing the number of nuclear localization signal (NLS) motifs within the Cas9 protein, they can enhance its ability to enter the nucleus, paving the way for more effective cell therapies.
This innovative approach, termed Hairpin Internal Nuclear Localization Signals (hiNLS), enables Cas9 to achieve editing efficiencies of over 80% in T cells, compared to just 66% using traditional methods. This is especially crucial for therapies like CAR T cells, which rely on precise gene modifications to combat diseases like cancer.
The study’s lead author, Christopher Doyle, PhD, emphasizes the importance of this discovery, stating that “enhancing nuclear entry could transform the landscape of gene therapy.” This marks a significant leap forward, as higher editing rates directly correlate with improved therapeutic outcomes and reduced production costs.
In their experiments, the Berkeley team tested their hiNLS-Cas9 variants on primary human T cells, targeting clinically relevant genes such as b2M and TRAC. The results were striking: using a peptide-mediated delivery method known as PERC, the team achieved knockout efficiencies of 40-50%, demonstrating the potential for broader applications in cell therapy.
This development is not just a scientific milestone; it carries profound implications for patients awaiting innovative treatments. As the manufacturing of cell therapies often struggles with consistency and yield, the improved efficiency of hiNLS-Cas9 could lead to faster and more reliable production processes, ultimately expediting access to life-saving therapies.
The implications extend beyond T cells. The researchers suggest that this method could also enhance the delivery of Cas9 to other hard-to-edit cell types, fostering advancements across various therapeutic areas. Moreover, the ability to produce hiNLS-Cas9 at scale without compromising yield positions it as a viable solution for clinical applications.
As gene editing continues to evolve, the potential for multiplexed approaches—targeting multiple genes simultaneously—grows more feasible with tools like hiNLS-Cas9. This could revolutionize the development of sophisticated cell therapies, offering hope to patients with complex genetic conditions.
Looking ahead, the research team is exploring complementary technologies, such as virus-like particles and lipid nanoparticles, to further enhance in vivo editing capabilities. The future of CRISPR technology is bright, and the implications of this advancement for global health cannot be overstated.
Stay tuned for further updates as this story develops, with potential breakthroughs on the horizon that could change the face of gene therapy as we know it. This is a critical moment in the pursuit of effective treatments for various diseases, marking a step closer to innovative solutions for patients worldwide.